I just came back from ASHP's Midyear Clinical Meeting and consider it a success. My experience was very interesting and reflects how crucial networking is for any interview process. From the airport to the actual conference itself, you should always be in interview mode.
Friday, December 10, 2010
The Importance of NETWORKING
I just came back from ASHP's Midyear Clinical Meeting and consider it a success. My experience was very interesting and reflects how crucial networking is for any interview process. From the airport to the actual conference itself, you should always be in interview mode.
Wednesday, December 1, 2010
Cancer Sucks!!

My fourth rotation was at Karmanos Cancer Center in Detroit. I was working mainly with patients in the bone marrow transplant clinic and saw most of them as outpatients. This rotation was extremely fulfilling in so many ways. I got to see on average twenty patients daily. Some of my duties included:
1. Meet with and counsel patients on each visit ensuring that medications are taken appropriately and updating their medication list.
2. Look for any drug interactions especially when patients were started on a new medication.
3. Most patients were either an allogeneic-transplant or an autologous transplant so I had to make sure that their medications were well correlated to the type of transplant.
4. Some other patients were pre-transplant so I had to make sure that these patients were not on any meds that would interact with their chemotherapy.
5. I also had to update vaccinations on these patients because after transplant, they are required to have vaccinations done on a schedule.
6. I was also in charge of noting every intervention made by the pharmacy team in the pharmD clinical notes.
This experience allowed me to hone my patient counseling skills. I also had the opportunity to build a relationship with these patients because I got to see most of them at least once a week. I enjoyed learning about the experiences they shared with me. I was impressed that most patients were very knowledgeable on all their medications.
My mother died of cancer. I never fully understood what she went through while she was battling cancer because I was young. However, now that I have worked with these patients and witnessed what they go through, I can only imagine what my mother went through. I have great respect for her and all other cancer patients and survivors.
Cancer sucks but we as pharmacists can work to help alleviate the pain that patients go through!
Monday, November 29, 2010
For my institutional rotation I chose a hospital close to home: Genesys Regional Medical Center in Grand Blanc. It wasn't the most exciting rotation I've had, but I think that can be said of most Institutional rotations. I managed to learn a lot, so I count it as a win!
Caring for the Critically Ill
I spent the month of November at Sinai Grace Hospital a place that I am very familiar with. I also intern at Sinai so I was very familiar with the surroundings and the staff, which made the month all the more enjoyable. My time at Sinai would be spent in the ICU’s dealing with critically ill patients. From the beginning I was told that to work in the ICU you have to look at it a lot differently than the general hospital population.
First, I had to realize that these were the sickest of the sick within the hospital and some of my patients were not going to make it. Secondly, I learned the goal of the ICU, which is to get the patient out of the ICU as fast as possible, the longer a patient remains in the ICU mortality increases. This differs from general hospital practice because you are to treat the patient’s main complaint or admitting problem. In the ICU the common admitting cause was shock secondary to pulmonary edema from pneumonia. This would develop while in the hospital or sometimes present to the ED with. More than any other problem pneumonia was most commonly seen in ICU patients. Pneumonia is so common in the ICU that any patient who presents with a spike in temperature or WBC and shows some sign of infiltrates on the CXR are treated empirically until sputum cultures return.
The ICU pharmacist we worked with throughout the month was also on the CODE team. His responsibility was to be present when a code blue (adult emergency) is called, and administer medications from the crash cart. The pharmacist would deliver the recommended doses of Epinephrine or Atropine as needed. During our first week we were fortunate to be present for a code blue. The room was filled with over 12 people of various medical disciplines trying to resuscitate the patient. Over 40 minutes later the patient unfortunately expired. It was a very gripping first experience at a code that I learned a lot from and will never forget.
By and large this has been my most enjoyable rotation to date. I think I enjoyed the ICU because of the fast pace that the teams work, and in part to the style of critical thinking that goes into determining the treatment plan for some very dangerous and rare conditions. While I was in the ICU I was able to learn about a lot of different and new treatment modalities. I would recommend that anyone who enjoys the fast paced work environment spend time in the ICU.
Sunday, November 21, 2010
Pharmacy Beyond "the Right Drug for the Right Patient at the Right Time"

Saturday, November 20, 2010
????!!!
I have spent the first half of November on rotation in the Drug Information Center at Ann Arbor’s Veterans Affairs hospital.
When VA staff members have medication questions they call the Drug Information Center. It is my job to provide answers to their questions. In a time when everyone on the medical team carries a handheld PDA full of downloaded drug information resources, the questions that make it all the way to me are the obscurest of the obscure. Questions like:
??!How do you prevent bortezomib-induced hypotension in a patient receiving hemodialysis??!
and
??!Is there any evidence for using minocycline to treat panitumumab-induced dermatologic toxicity??!
The great thing about the drug information center is that so many excellent drug information resources are readily available. They have some of my personal favorites; Lexi-comp, Micromedex, Facts & Comparisons, PubMed with full text access, Trissel’s and plenty of conversion and compatibility charts. So when I get puzzling questions like these I am able to find the answers if they are out there.
Most of the questions people ask do not require immediate responses, so I am usually given plenty of time to come up with thorough answers. It’s a great way to help out in caring for patients, in a mellow environment. I can see how drug information would be an attractive field for the pharmacist who is interested in research and caring for hospitalized patients, but wants to avoid the hustle and bustle of the floor.
Saturday, November 13, 2010
Ghana International Rotation
I have traveled to Ghana several times in the past with my family, and this experience was vastly different from the others. The first and most notable difference was that this was not a vacation and that I would be working at Komfo Anokye Teaching Hospital (KATH). Although I had traveled to Ghana several times prior, I had my first ride on a Trotro. This was by far the new experience outside of KATH that I will remember the most. I had always wondered how the Trotro system works and how you would know where each Trotro was headed, now I know. It was a bit of an adventure the first time I had to wait at Tech Junction with close to 50 other people waiting to head into town. The moment the Trotro pulled up and the doors opened there was a mad dash to the doors to be one of the 12 fortunate people who had a seat, and avoid having to wait another 20-30 minutes for the next one. Although we ended up taking a droppin the rest of our time in Ghana, the Trotro experience is one that I will always remember due to its authenticity to Ghana.
My experience at KATH was just as memorable. KATH on appearance seemed very different from the hospitals I had experienced in the past. As the saying goes “appearances are only skin deep”. As we began to round with the pharmacists and the clinicians, I realized that a lot of the same types of patient and administration issues were present. KATH services a lot of patients in a very resource-constrained facility. Although the budgets may be different hospitals everywhere are faced with the burden of trying to deliver the patient the best care possible, while keeping their costs down. The issue of medications that are too expensive for the patient to afford arise often in the US and similar to here it is up to the pharmacist to determine an alternative medication that has similar efficacy that the patient can afford. Some similar patient issues that I encountered were patients who were non-compliant when it comes to regularly taking their insulin or other medications. It was up to the pharmacist and other health personnel to try to convince the patient of the importance of compliance and how properly taking the medication would lead to less hospital visits.
Another similarity that I was surprised to find is that both Hypertension and Diabetes are very common disease states. I believe that the diet plays a large part in the prevalence of diabetes in Ghana. The diet is filled with dishes heavy on carbohydrates and low on green leafy vegetables. These posse a large problem when attempting to counsel patients on their diabetes and lifestyle changes that needed to be made to improve or slow the progression of the disease. Patients with Hypertension often came to the hospital with very high initial blood pressures. The pharmacists attributed this to patients’ unwillingness to receive frequent check ups. By the time the patients come to the hospital the condition had worsened and would take longer to stabilize. Both of these conditions and issues often occur in the US as well.
Some of the differences that I noticed immediately while on the wards were the prevalence of different infectious diseases. Disease states such as malaria, enteric fever, tuberculosis and schistosomiasis are things we read about but only if we are lucky would we ever encounter it in the hospital. Another disease state that I had never even heard about but is endemic to the area was Buruli Ulcers. I was very surprised to learn of how common it was, so much that the World Health Organization sends a lot of resources and support to help prevent the spread.
I have truly enjoyed this trip to Ghana and getting to experience the country from a new perspective. Being a Ghanaian-American this trip has opened my eyes to some of the woes of the health care system and limited access to resources, be it health based literature or actual medications.
Sunday, November 7, 2010
Committed to Mental Health
My current rotation is at Pine Rest Christian Mental Health Services in Grand Rapids, MI. It's a psychiatric inpatient unit, meaning the patients are a potential danger to themselves or others. Needless to say, the interesting patients are one of the best parts of the rotation.
I've seen most of the major psychiatric conditions, and many times patients have more than one diagnosis. I've seen patients hospitalized for major depression, bipolar disorder, schizophrenia, mood disorders, substance abuse, eating disorders, and post-traumatic stress disorder. Some of patients with psychoses are very insistent that what they perceive is real, while others have very good insight that what they are experiencing is a symptom of their disease.
Aside from the interesting patients, there are some other perks to the rotation. There is only one clinical pharmacist for the entire facility, so I get to participate on all pharmacy consults. That also means that he is the lone pharmacotherapy expert on the team and his opinion is well-valued.
In terms of pharmacotherapy, I am learning a lot. Because of the long-term nature of these conditions, stopping therapy is not an option (and is often not legal due to court orders). As a result, psychiatry is one area where we do try to treat side effects with additional medications. It's also an area where different drug forms are of high value. For example, decanoate injectable forms of drugs are useful because they allow us to achieve therapeutic levels with monthly or every two week injections as opposed to daily oral therapy. In a patient that has compliance issues, this is a great option. We also turn to liquid or orally-disintegrating tablets in certain patients that have been known to hide a tablet under their tongue to spit it out later. This is sometimes an issue in paranoid or manic patients.
So far, I've really enjoyed my rotation at Pine Rest. The patients are interesting. The medication therapy is interesting. I also feel that the facility is run in a very safe and humane way. If you're interested in psychiatry and have a place to stay in Grand Rapids, I can certainly give this rotation my recommendation.
Tuesday, October 26, 2010
"Dark and early" at the Trauma Burn Center
Last Friday, I completed my first inpatient rotation- Trauma Burn. My main reason for choosing to take this rotation was because of my PharmD investigations project which looks at the use of an anabolic steroid in burn patients. If there's one thing I hear frequently about this rotation, it is "rounds are early". Indeed, rounds are very early; starting at 6am on most days and at 5.30am every Thursday. Hence, before I go to bed the night before, I need to have a good idea of the issues I like to bring up on rounds. On most days, I would arrive ~15 minutes before rounds begin to look up some labs that came back overnight. This is also the time when the intern on-call last night gives report to other interns, so sometimes I can get an idea of what happened to my patients overnight even before rounds begin.
In many ways, this was the hardest rotation I've had so far. Yet, it was also my favorite because I gained so much clinical knowledge and developed a more systematic way of looking at patients. Here are 3 main learning points that I hope to share:
1) Be at where things happen.
When you are on inpatient rotations, try to be on the unit as much as possible. There are "COWs" (computer on wheels) along the hall which you may use to work up your patients. In this way, you see what happen to patients, you hear what interns/residents say, and you get the latest updates. When the interns see you around, they ask you questions (eg. antibiotic dosing). You feel involved and they see you as part of the team.
2) Be ready when you make a recommendation.
Whenever you make a recommendation, give a rationale. If you propose adding a new drug, have the dose ready and be sure you can explain your choice and give your reference (if applicable). By being ready, you sound more credible and that increases the likelihood of your recommendation being accepted.
3) Persistence counts.
If your recommendation is not accepted the first time, keep bringing it up when similar situation arises. I encountered a situation on BICU rounds where the chief resident changed IV ranitidine to PO omeprazole whenever patients were able to tolerate oral medications. The reason being PPIs are "innocuous" and Zegerid can be dissolved in water and be administered easily down a tube. It wasn't until the third time that I bring up this issue that he was willing to listen to my explanation of why the H2RAs are first line for stress ulcer prophylaxis (VAP, C. difficile, etc.) plus ranitidine comes as a liquid. He was convinced! So persistence counts and being able to explain the rationale behind your recommendation counts. Even if your recommendation was never accepted, take it as an opportunity to educate and demonstrate your knowledge!
Monday, October 25, 2010
"Words Can't Bring Me Down"
After driving eight hours, I am now sitting at home in St. Louis, Missouri, waiting to start my fourth rotation at Facts and Comparisons. During my drive, I was listening to my Glee CD that I got from my roommate when something sort of inspirational happened-the song “I am beautiful” came on. Most of you have probably heard of this song. I never really paid too much attention to the lyrics until yesterday. When she sang “words can’t bring me down,” it brought up the memory of an unforgettable incident that occurred to me during my second rotation in an outpatient oncology clinic.
As part of my routine work at this clinic, I sat down with patients to go over their medications to make sure that our medication list was reflective of the patients’ most current medications. This process, called medication reconciliation, is an important step in taking care of our patients. Each time a medication reconciliation was performed, I checked to see if there were any clinically significant drug-drug interactions, whether the dosages were correct, and if each of the medications had an appropriate indication. Equally important, I asked my patients if they took any supplements or over-the-counter medications. If my patients were on a pain medication, I would inquire the specifics as to how many pills were taken and how often they took them. In addition, I inquired about how well the pain was being controlled.
One morning, as I sat down near my next patient with whom to conduct a medication reconciliation, I felt an unwelcoming atmosphere from her nonverbal body language. I quickly dismissed this thought and began my usual routine of performing a medication reconciliation. Similar to what I did with other patients, I introduced myself and explained my role. Then, when I asked her “Do you still take drug X?” and “How often do you use this medication?” she abruptly raised her voice and said, “What is the point of asking all these questions?” I was taken aback with this sudden outburst of discontent. I looked to her husband sitting to the left of her, who did not seem perturbed. I re-focused back on her and explained to her the importance for us to have an updated list of all current medications, especially since she was receiving chemotherapy. My explanation did not work. She stated that she would continue this process not because she saw benefits in it, but because it was an educational opportunity for me as a pharmacy student. Feelings of intimidation and the uninvited atmosphere overwhelmed me during these brief few minutes. Seeing that further explanation would be futile, I quickly recollected myself, thought about my original intention of performing a medication reconciliation, and went ahead and continued the interview to make sure that all pertinent questions were answered. Even though this was not the most pleasant interview, I tried not to let her “words bring me down” and maintained my professional demeanor. When we were finished, I politely thanked her for her time.
As I am writing about this incident, my patient’s words and expressions are still clear in my mind. Though it was not a pleasant experience, this is a part of life. Even with the best intentions, people are sometimes wary of your actions. Even I must be guilty of this at times. As health care professionals, we work in a helping industry, and no matter how our patients perceive us, we are here because we want to help others. The lyrics, “words can’t bring me down,” serve as an encouragement and inspiration for me to continue to believe in the work that I do. Looking at this event retrospectively, I am thankful that my patient allowed me to gain this insight and to grow from the experience. When else is a better time to experience setbacks and unpredictable events than now?
Saturday, October 23, 2010
Serving the COMMUNITY
.jpg)
Working at THE Pharmacy, Ypsilanti has been very great and eye-opening experience. Contrary to popular belief, not all community pharmacies work hard to fill and dispense scripts without focusing and addressing direct patient care. I started to make interventions on day 1 of my rotation. For example, a customer complained that her Children’s Multivitamins that she bought at The Pharmacy had black spots. My preceptor (Kiela Samuels, PharmD) brought the situation to my attention and asked that I called the manufacturing company. I did so and the company explained that the vitamins may have been turning black because the product contained iron and iron coming in contact with moisture leads to oxidation and consequentially, to the black spots forming on the vitamin tablets. They offered to send the dissatisfied customer a coupon in the mail for a replacement bottle. I felt accomplished because I learned something new and the customer was also satisfied in the end.
This experience made me pumped to do more and learn more about how I could make a difference at the pharmacy. I performed several blood pressure measurements daily and gave useful recommendations in my first week. I also applied what I learned in my previous rotation to this rotation. I had my inpatient cardiology last month and I learned a lot about meds for cardiovascular diseases so when I saw that a patient with chronic heart failure was on metoprolol IR, I immediately though why not ER as shown in the MERIT and COMET trials. I brought this to the pharmacist’s attention and we had a discussion as to why the patient was not on ER with the patient’s daughter. The feeling of being able to apply my previous learning was elating and this motivated me even more to screen patient profiles and intervene whenever I could.
I got involved in many other things at my rotation. Some of these things include:
1. The Antibiotic Call-Back Program
Everyday, I have a list of patients that I had to call to follow up on how their antibiotics were working for them. As little as it may sound, it makes such a huge difference because these patients appreciate that we are concerned about their health. They also appreciate the effort made to call to check up on them. It helps to build trust and confidence in the pharmacist in the long run and these patients feel more comfortable in confiding in the pharmacist.
2. Constant Med Profile Reviews
We constantly check to see how patients are doing when they get their refills. We also set time out to counsel patients and ensure that they understand why they are taking their meds, what to monitor for and goals to expect upon proper compliance and use of the drug.
3. Compounding
I also got to compound medications at the allergy clinic every Thursday. I got a lot of practice in compounding and can say that I am now proficient in compounding mixtures ☺
4. Teaching
Every Thursdays, I was like a teaching assistant to Dr. Samuels at the Washtenaw Community College. She was involved in teaching students in the certified pharmacy technician’s program. I got to see what it was like from the technician’s view. I really valued this experience because most pharmacists have to work with techs and this experience helped me to see what it was like for them to learn the skill they have to apply in pharmacy.
There is so much more that I can share but overall it was a great experience! You can always email me with questions and I will respond as soon as I can…
Tuesday, October 19, 2010
Drug Interactions- Wading through the data
For my third rotation, I have been working on drug information with LexiComp. My preceptor works specifically on all topics related to drug interactions, including writing the monographs seen in LexiInteract.
Why is everyone talking...
about poop?
Tuesday, October 12, 2010
A Part of the Community
This month I am on rotation at an independent retail pharmacy called Warren Sav-Mor Prescriptions. You might be surprised to learn that it is not in Warren, MI but rather on the border of Farmington Hills and West Bloomfield. The Warren part of the pharmacy's name comes from its long history as an independent pharmacy owned an operated by the Warren family. Sav-Mor is a conglomerate of independently owned pharmacies in Michigan. Sav-Mor gives these independent pharmacies some tools, like a computer system and some supplier contracts that allow them to compete against the big corporations.
When I think of an independent pharmacy, I typically think of a low-volume niche type store. That's not how this store is... they fill up to 500 prescriptions on a busy day. During my rotation, I have discussed the business aspect of an independent pharmacy quite a bit with my preceptor. Because he is so involved with the business-side of things, sometimes he will straight-up tell a customer "Look, I buy this at $45 for 30 pills. I'm not even making any money off of this." He's telling the truth, too, and the customers are often more satisfied after hearing that. Both my preceptor and the other main pharmacist at Warren have worked there for more than 20 years: they know retail pharmacy and the business side of it inside and out.
I've seen polls where pharmacists were perceived as one of the most trusted professions in communities. Now I can see it with my own eyes. Of course people get angry when there is disconnect between the prescribers, insurance companies, and pharmacy, but they listen to what the pharmacist has to say. For good reason, too: When I ask some of the customers if they've filled prescriptions there before, some answer "Yes, you must be new. I've been coming here for 20 years now."
Monday, October 4, 2010
Rotation 2: Arrhythmias, Heart Failure, CAD, Hypertension and the list goes on!

After going through my cardiology rotation, I can gladly and proudly say that I learned a great deal within the short time span of a month. My rotation was at the University of Michigan Hospital. My typical day involved me waking up at about 5am to work-up my patients then head off to the hospital for early morning rounds. After rounds, we would meet with our preceptor to discuss all the patients that we rounded on, usually focusing on their drug therapy and medication plans. It took me a while to blog about this rotation because I have so much to share so I tried to condense it as best as I could. Feel free to contact me for more info/questions.
Here are a few pertinent things I learned.
1. In dealing with patients, focus on drug therapy!
When rounding with a medical team, it is easy to get sucked into all their recommendations for patients with regards to their drug therapy. Most times, the medical team is right about choosing medications for a patient but they do not always choose the best medication for a specific patient. We are pharmacists in the making and our job is to make sure that every patient is on the best medication for their disease state. These include accounting for drug interactions, therapeutic duplications and disease state. While on my cardiology rotation, I learned to look at each patient’s condition and ensure that they were on all the right medications without being influenced by the medical team’s decision.
2. Don’t sleep on Evidenced Based Medicine (EBM) and Keeping up with Literature!
This rotation provided the opportunity to go through over 100 important journal articles/reviews in cardiology. I was able to connect groundbreaking studies with recommendations for drug therapy. For example, according the 4S Lancet trial, we know that any patient with coronary artery disease (CAD) should be on a statin. I would go through patient’s profile and ensure that they were on a statin and I found myself making an intervention/suggesting a statin to the medical group on more than one occasion. Additionally, if a patient had A-fib, I will be checking to make sure he or she was on warfarin and also ensuring that he or she was followed by an anticoagulation clinic as an outpatient to monitor their INR. These are a few of the interventions I made on a daily basis.
3. Science is always evolving!
Like many other sciences, pharmacy and therapeutics are always changing. To be the best pharmacist you can be to a patient, it is therefore important to stay up-to-date with literature and drug-related issues. My preceptor was a very good role model because he was very current with pharmacy and drug related issues not only pertaining to the field of cardiology. One advice he gave that resonates with me all the time is to continuously educate myself even after graduating from pharmacy school. It is very easy to say that we would try to stay current with the information but when we get out to the work force and have other responsibilities, it is easy to get swamped and forget to keep up with continuous education. This is something I am going to be very conscious of and I advice my fellow students to be conscious of this too!
Overall, the rotation was awesome. I learned a great deal and I am very happy I had it early on in the year because I feel more prepared for my other rotations!!!
Tuesday, September 28, 2010
Non-Trauma Emergency (NTE)
When I first learned that I had the non-trauma emergency rotation I was excited because I knew I was going to see all sorts of interesting things. The more I thought about it I became more and more uncertain of what I was going to experience because I had no clue as to what exactly was a non-trauma emergency. To put it as concise and simple as I can its really any kind of Gastrointestinal surgery that needs to be performed immediately. The best example I can give is someone has appendicitis and needs an appendectomy immediately; they would be placed on the NTE service.
When this rotation first started the adjustment that I was most concerned with was not learning all the various surgical procedures and treatments. I was concerned with how my body would adjust to having to be at the hospital and ready to go at 5:30am some days earlier. I have never had to be up so early for an entire month, but after the 1st week I can say I hardly even noticed the time.
The thing I enjoyed the most about this rotation was that 90% of what we were doing was completely new which required a lot of on the spot learning. It also gave me the opportunity to better acquaint myself with the anatomy of the GI system. I’m sure your wondering what exactly the pharmacist does on an NTE rotation so let me begin.
We would arrive at 5:30 or 5:45 to round with the NTE surgical team which consisted of 3 residents, 2 Physician Assistants, a few medical students, and the pharmacy staff consisting of Dr. Kraft, Jason, and myself. While rounding we would discuss the clinical plan for patients with problems ranging from Appendicitis, Pancreatitis, Choledolithiasis, Fistulas and Ostomys. The team would discuss the the best surgical plan, medication plan and even the best nutrition plan for the patients. I was pleasantly surprised at how often the team would look to the pharmacist for information about various medications and nutrition in the patient. Total Parenteral Nutrition (TPN) is a very important aspect of a patients care plan if they want to recover. I realized that a lot of times when patients have GI issues they are incapable of consuming there nutrition by mouth so it must be administered IV. It is up to the pharmacist to make sure that the patient receives the right amount of fluids, protein, carbohydrates, lipids, and electrolytes to restore their health, because a large majority is malnourished. Nutrition happens to be a good indicator at the likely hood of having a successful surgical procedure. Patients with very poor nutrition status were sometimes withheld from surgery to improve there nutrition to increase they chances of recovery post surgery. All in all this was a very beneficial and informative rotation. I learned a great deal about GI surgical, and infection issues.
Call Me Beep Me if you Wanna Reach Me...
Rotation #3 for me is drug information at U of M. Today I worked the call center and had some interesting calls....
A nurse practitioner (NP) called explaining how a patient reacted to spironolactone with rash and hives. She was wondering if the patient could be switched to eplerenone, which is also an aldosterone antagonist. The NP had concerns about cross-reactivity between the 2 agents. Patient can tolerate furosemide, and also has a sulfa allergy.
So I proceeded to search Micromedex, Lexi-Comp and PubMed to find any information about aldosterone and eplerenone cross-reactivity. No mention about cross-reactivity. Then I recalled the patient has sulfa allergy so decided to search that term in the monographs of the 2 drugs. I saw spironolactone has metabolites containing sulfur...so then I thought, "OH! that's why the patient had a reaction" Then...I proceeded to look at Goodman & Gilman to look at the STRUCTURES of aldosterone and eplerenone. Turns out aldosterone contains a sulfur atom, and eplerenone does not. I discussed my findings with my preceptor and we came to the conclusion that switching from aldosterone to eplerenone should be safe.
So what's the point of my story?
My knowledge gained from the medicinal chemistry courses actually came to use! In my formal write up to the NP, I was tempted to be a geek and write about the "sulfur moiety of the chemical structure"...but I just stood with saying "sulfur atom in the structure."
To be honest, I was intimidated at first to take phone calls to answer drug information questions mainly from other health professionals. However, I am finding it fun because people call asking for your advice. I research the question asked, then I follow up, and the caller is really grateful for the help...it's a great feeling to be a great source of information. I am also learning things I don't think I would otherwise know. For example, I learned today that the Fluvirin vaccine is stable in 77 degrees fahrenheit for up to 72 hours after 1 excursion. Pretty random, huh?
Monday, September 27, 2010
I have always appreciated the importance of research and how it translates to the standard of care at the bedside. A PharmD Investigations Project, which gives pharmacy students research experience, is a unique component of the U-M PharmD program. We get to pick an area of interest and to conduct a guided research project, from writing a proposal, to doing the actual project, and then presenting it in a seminar setting. Students also have the option of presenting a therapeutic topic for their seminar if they so choose.
I had the pleasure of working with Dr.
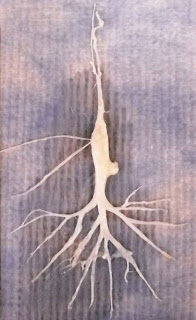 Stringer for my project. It is focused on a rare but potentially fatal pediatric condition known as plastic bronchitis. Its hallmark symptom is the formation of thick, rubbery, bronchial casts that take the shape of the airways where they are formed (see photograph). My project is on supporting the use of inhaled tissue plasminogen activator, a fibrinolytic approved for myocardial infarctions and strokes, in this patient population. Dr. Stringer has challenged me to think about research topics critically as well as given me great advice on presenting a research topic.
Stringer for my project. It is focused on a rare but potentially fatal pediatric condition known as plastic bronchitis. Its hallmark symptom is the formation of thick, rubbery, bronchial casts that take the shape of the airways where they are formed (see photograph). My project is on supporting the use of inhaled tissue plasminogen activator, a fibrinolytic approved for myocardial infarctions and strokes, in this patient population. Dr. Stringer has challenged me to think about research topics critically as well as given me great advice on presenting a research topic.As the first student to present my PharmD seminar in my class, I felt stressed about the limited time to prepare. In response to my nervousness, Dr. Stringer said, "We are going to set the bar high!" and "I will do everything I can to make sure you do great on your seminar." Both comments were very reassuring. I delivered my seminar successfully on September 24. In retrospect, I could have prepared a little more for the Q&A session. Here are some tips I can offer anyone who is presenting a seminar for the first time.
- Start preparing as early as possible. If you have a rotation that is less demanding, start now! It will take longer than you think.
- Think of your seminar as telling a story. Give your audience enough details to understand the material. But also remember to keep it "simple and stupid."
- State off the bat why your topic is important, so your audience know why they should pay attention to you.
- Keep your slides simple. Try to follow the "7 (words across) by 7 (rows down) Rule." Your slides are just a tool that supplements your verbal presentation, not take the place of it.
- Practice, practice, and practice. Use tone of voice, pauses, and choice of words to inspire your audience and keep them interested.
- Use visuals. We are all visual creatures and a picture is worth a thousand words.
- Preparing for anticipated questions will make you less nervous during the Q&A session!
- Choose an advisor whose work habits match yours. I am very happy and very fortunate to have an advisor who is very attentive to my areas of improvement and is patient enough to teach and guide me. I could not have completed this seminar successfully without her.
Sunday, September 26, 2010
The Wonderful World of Warfarin
I spent the month of September in the transitional anticoagulation clinic at Sparrow hospital in Lansing.
I liked anticoag. It was a good mix of the outpatient and inpatient settings.
I spent the first half of each day in the clinic, seeing patients who had recently been hospitalized at Sparrow with new prescriptions for Coumadin. I read their INR, spoke with them about the importance of adherence, and we discussed Coumadin’s most common drug and food interactions during 15 minute appointments.
Since the patients were just getting started with Coumadin, we saw them frequently to make dose adjustments. It did not take long to get to know everyone who was a patient at the clinic.
I spent the second half of each day speaking with patients who were still hospitalized and ready to be discharged with new Coumadin prescriptions. I discussed Coumadin and low-molecular weight heparin with each new patient for about an hour, and they often had many questions. I remember being pretty nervous the first time I had to run one of these counseling sessions on my own. By the end of September the long sessions were my favorite part of the day.
I have always worked in inpatient pharmacy so being able to interact with the people I was taking care of was a new experience. It was rewarding being able to see patients’ health improve from week-to-week and knowing that I was contributing to that improvement.
Saturday, September 25, 2010
In the CUB Unit
This past month I was at Allegiance Health for my inpatient cardiology rotation. I spent my time at the CUB (cardiovascular universal bed) unit monitoring patients from the time they have open heart surgery until discharge. To get a better understanding of what patients go through, I was given the opportunity to observe a CABG (coronary artery bypass graft) and aortic valve replacement surgeries! I thought I would pass out from seeing all the blood and organs, but was able to keep my cool.
As I reflect back, some thoughts that stick out in my mind:
(1) P-care discussion sessions linked with Institutional & Community IPPE: Extremely valuable! In these discussion classes we are assigned to work up patients and give patient presentations. All those long hours I spent last year working up patients has paid off. Working up patients on P4 rotations is nothing new since I got good practice during P3 year
(2) You still need to know everything! Although I was doing a cardio rotation, non-cardio issues arose such as delirium and aminoglycosides dosing
(3) Utilize your fellow health
(4) Try extremely hard to have most of your PharmD investigations project complete prior to P4 rotations- Rotations are busy...on top of your tasks during the day on site, you also have to work on presentations for rotation pretty much each week. Such workload gets done when you get home from a 7-10 hour day at rotation. This past month I have been working on my P680 Seminar as well, which is a huge presentation you give 4th year on a topic you have to research extensively. At least have your data collection and analysis for PharmD investigations project complete since it's 1 less thing to worry about.
After completing this rotation, I feel like I have further developed my clinical skills. My mind automatically clicks what drugs and important lab values to look for in a patient undergoing cardiac surgery. I have also identified areas in which I need improvement. For future rotations I hope to work on these weaknesses and better fine tune my skills.
